Please read the Declaimer before reading an article/ content on the website
About the author
This article has been kindly written by Dr. Rebecca Moore from the United Kingdom. Dr. Moore is a renowned Perinatal Psychiatrist working in London, with experience spanning over twenty years. Her role incorporates working with and supporting women who have new onset or pre-existing emotional issues through pregnancy and up to a year after birth.
Dr. Moore worked with one of the pioneers of Perinatal Psychiatry, Dr. Liz MacDonald as a trainee in London (UK), and she was inspired to pursue work in the field.
Dr. Moore is passionate about her job and has developed a particular interest in birth trauma.
Dr. Moore is also training to be an integrative practitioner and uses exercise, diet, movement and meditation and stress management as key parts of her treatment approach.
To find out more about Dr. Moore’s work, please visit www.doctorrebeccamoore.com or connect with her on Instagram (@drrebeccamoore) or Twitter (@dr_bjm)
Birth Trauma
What is birth trauma?
Birth trauma occurs when women find some aspect of their birth traumatic, distressing, and/or fearful.
It doesn’t matter what the woman finds difficult, it’s your birth experience and if something felt hard, frightening, scary or out of control that’s your story.
Statistics to remember
Currently, around 30% of women find some aspect of their birth traumatic, which equates to over 150,000 women per year, that a lot of women starting the journey to motherhood feeling really difficult emotions.
Yet, birth trauma is not well recognised or identified.
Additionally, leaving birth trauma untreated in the long term can lead to enduring health repercussions both for mum and her family.
Not all women who have a difficult birth go on to develop Depression, Anxiety or Post Traumatic Stress Disorder/PTSD, However, some will.
Where women have a history of prior anxiety, depression or sexual abuse, 1 in 5 of this group of women will develop Post Traumatic Stress Disorder after birth.
Communication and Care matters…
Trauma at birth encompasses more than life-threatening medical emergencies such an emergency Caesarean births or a heavy bleeding, just as often it can be about the care and language we give to women in labour.
This may mean women being spoken about not to, ignored or dismissed by staff, and feeling unheard or not listened to. It may be a lack of kindness or care, staff not introducing themselves or not respecting the woman’s wishes during birth, or women feeling coerced during labour.

Let us take two examples to understand the situation better (Both of them are imaginary situations used for educational purposes and not real-life cases and any resemblance is purely coincidental):
1. Mrs. X who comes into delivery knowing her midwife and having had lots of antenatal discussions about her birth preferences. She then has a long painful labour ending in a Caesarean birth and a postpartum bleed.
She perceives her birth as positive, despite it not being the birth she hoped for.
She had someone by her side throughout explaining to her what was happening, reassuring her, allowing her to raise concerns and fears.
This helped in sustaining a sense of control and choice, including, for example, immediate skin to skin after birth in theatre.
Therefore, although Mrs. X had medical intervention and complications, she had a positive experience of birth and did not develop birth trauma.

2. In a different scenario, Mrs. Y comes onto a busy ward to meet a midwife she does not know who is courteous but not especially warm. The midwife keeps leaving the room for long periods of time and she is increasingly worried that her labour is progressing quickly and she might deliver on her own.
Mrs. Y feels out of control and scared. She does not get a chance to ask about pain relief much and by the time she asks for an epidural, which she wanted, she is told it is too late.
When the baby is born he is placed on Mrs. Y’s chest immediately uncleaned, which she did not want, and when she asks the midwife to take the baby and clean him the midwife makes a comment to Mrs. Y – “that’s unusual”.
Mrs. Y then transfers to the postnatal ward where everyone comments on how lucky she is to have had such a fast birth but she doesn’t feel very lucky or happy.
She starts to ruminate about what the midwife said, doesn’t sleep all night, feels guilty about not having her son on her chest immediately after birth.
Mrs. Y has a rapid four-hour vaginal birth with no complications or medical intervention, she also has trauma from her birth experience.
Dads do suffer too…
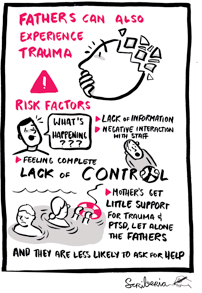
It is important to recognise that fathers can be traumatised by birth and that midwives, students, doulas in the room can also be traumatised.
What are the symptoms?
Postnatally the focus is often on the baby and on a mother’s feeding, bleeding or Depression.
Persistent all day long sadness, tearfulness, low mood, anxiety, fatigue, and loss of enjoyment in life, can all indicate depression.
In post-traumatic stress disorder or birth trauma, we would expect variable mood, fluctuating from sad to angry to tearful to guilty.
This usually occurs alongside recurrent overthinking or replaying of the birth in dreams, thoughts or visual flashbacks of moments including a comment made, a doctors’ face, blood on the floor, or the baby not crying after delivery.
Women often feel unable to relax or on edge all the time and may be overprotective of their baby or check on their baby all the time. Women often find it hard to hear other people’s birth stories or see other pregnant women or small babies.
What can be done to help the mothers/ parents?
Healthcare professionals should meaningfully ask all women how their birth experience was as part of routine care. This could be as they leave the maternity ward, by their health visitor or at their six-week postnatal check.
We need to give women enough time to talk through their feelings and tell their story and to know we are really listening and hearing them. Many women dismiss their feelings or feel guilty talking about their birth experience.
It is possible to have a bad birth experience and still be a good mother and love your baby very much and we must allow women the space to process their birth. A healthy baby is not all that matters!
Often women are never asked about their birth story and so these traumatic feelings and emotions remain. I have met women in their 70s who have told me about their birth trauma for the first time.
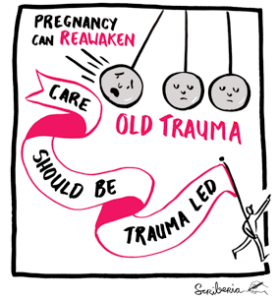
Commonly, I encounter a woman in a second pregnancy with undiagnosed post-traumatic stress disorder for years as result of her first birth.
It is not uncommon for women to never have another child because their birth experience was so traumatic.
Speaking to others could be helpful…
If women feel traumatised by birth we should encourage them to feel able to speak to someone they trust, a partner, friend, midwife, health visitor or general practitioner.
However, talking about the birth-trauma could sometimes be challenging. Therefore, if this is over-whelming women can be encouraged to try and write down their story in a blog or use a journal.
Online forums can be very helpful as it allows women to speak anonymously, this might be via twitter or a peer group forum.
Various other factors can help birth trauma, such as diet, exercise, sleep, social support, meditation, breathing, psychological or physical therapy and/or medication.
The prognosis is very good once identified and most women feel significantly better within 12-18 months with the right care.
It can seem never-ending and terrifying to be traumatised by birth but women do get better and we must always try to engender hope about recovery.
NICE Guideline (CG192) published in December 2014, suggests that if someone develops Post Traumatic Stress Disorder (PTSD) following childbirth, then she should be offered trauma-focussed Cognitive Behavioural Therapy (CBT) or eye movement desensitisation and reprocessing (EMDR).
Birth Trauma Resources
1. Annual Birth Trauma Conference run by Dr. Moore in East London (UK) every year in December. This is free to attend, to be booked directly with Dr. Moore (please contact her on the above details or visit her website for further details). The next Conference would be in 2019.
2. Perinatal Psychiatry, Birth Trauma and Perinatal PTSD: An Interview with Dr. Rebecca Moore
3. When Birth is Trauma: a guest post by Elizabeth Ford on MidwifeThinking website.
4. Solace for Mothers: Healing Birth Trauma.
Research Papers
1. Wijma K, Soderquist J, Wijma B. Posttraumatic stress disorder after childbirth: A cross-sectional study. Journal of Anxiety Disorders. 1997;11(6):587-97.
2. Czarnocka J, Slade P. Prevalence and predictors of post-traumatic stress symptoms following childbirth. British Journal of Clinical Psychology. 2000;39:35-51.
3. Ayers S, Harris R, Sawyer A, Parfitt Y, Ford E. Posttraumatic stress disorder after childbirth: Analysis of symptom presentation and sampling. Journal of Affective Disorders. 2009;119:200-4.
4. Ford E, Ayers S. Support during birth interacts with prior trauma and birth intervention to predict postnatal post-traumatic stress symptoms. Psychology and Health. in press.
5. Soet J, Brack G, Dilorio C. Prevalence and predictors of women’s experience of psychological trauma during childbirth. Birth. 2003;30:36-46.
Websites
1. Birthtalk.org (Australian)
2. Make Birth Better (UK website mapping out local geographical resources for birth trauma)
3. Birth Trauma Association. Has some good links to phone lines/peer group forums.
4. Mat Exp Facebook group http://matexp.org.uk, a wonderful forum for professionals and those with lived experience to safely and respectfully ask any kind of question about maternity, promote the best practice, events. Highly recommended and a very inspiring innovative group.
5. Positive Birth Stories http://www.positivebirthstories.com, feedback about positive birth experiences
6. http://tellmeagoodbirthstory.com, feedback about positive birth experiences
7. http://www.rcgp.org.uk/clinical-and-research/toolkits/perinatal-mental-health-toolkit.aspx, a fantastic overview of all aspects of perinatal mental health including birth trauma, UK based.
Books
1. ‘How to heal a Bad Birth’ by Brujin and Gould.
3. Why Human Rights in Childbirth Matter by Rebecca Schiller,
4. Fine (Not Fine): Perspectives and Experiences of Postnatal Depression by Bridget Hargreave
5. Heal Your Birth Story: …releasing the unexpected by Maureen Campion
6. Moods in Motion: A colouring and healing book for postpartum moms by Karen Kleiman, for some women art, journals can really help birth trauma and this is a lovely colouring book that can help anxiety, promote mindfulness.
7. Cognitive Behavioral Therapy for Perinatal Distress 1st Edition by Amy Wenzel (Author), Karen Kleiman
Apps
1. Peanut/ Mush (UK based to meet local mums)
2. Calm/Headspace Meditation Apps
1. @Mumologist (clinical psychologist, feminist, birth trauma expert)
2. @Suzy Reading (information on self-care)
3. @Mothers.Wellness.Toolkit (discussion on motherhood, and especially pelvic care/Pilates)
4. @Wild Fig Nutrition (postnatal nutrition)
5. @When the Bough Breaks (on maternal mental health, US-based)
Please read the Declaimer before reading an article/ content on the website

