There is increasing interest in meditation with regards to the prevention and treatment of different health conditions. This article briefly outlines the science behind the meditation in the light of research evidence. We also discuss the different health benefits and possible risks with this practice.

What is meditation?
The word ‘meditation’ comes from the Latin word ‘meditari’. This means ‘to think’ or ‘to contemplate’. (Ref)
The aim of the meditation is to achieve a ‘thoughtless awareness’ mental state (‘mental silence’), where the mind is calm, peaceful and free of any automatic thoughts (‘mind wondering’) and internal dialogues (‘mental clutter’).
This leads to both physical and mental relaxation. Meditation is also believed to improve the regulation of the emotions and a balance of the mind. (Ref)
This peaceful mental state and relaxation cannot be achieved through sleep or other deep relaxation techniques alone.
Meditation, therefore, is different from sleep and other relaxation strategies.
Researchers believe that the meditation originated several thousand years ago in India and found descriptions in the Vedas (ancient Indian scripts). (Ref)
At present, there are various forms of meditation practices within different cultures and religious beliefs. (Ref)
Although there are many different types of meditation practices, the three basic principles of meditation are:
1) To concentrate:
One of the main goals of meditation is to improve the concentration and attentional skills.
This involves either of the following –
– Focussing the attention on breathing, an external object/ point in space, or chanting of a mantra (the examples are Sahaja Yoga, Yoga Nidra, and different religious prayers)
– Focussing the attention of the mind non-judgementally at the present moment (such as Mindfulness). (Ref)
2) To bring the attention back if distracted:
Meditators observe the mind closely if the focus of concentration is wandering off.
If this happens, the meditator would need to bring the attention back to the focus of concentration.
3) Open monitoring of the mind:
This involves observing all the thoughts coming to the mind (both automatic thoughts and in response to external events) closely in a non-judgemental way. Therefore, they do not actively respond to any thought.
It has been observed that practicing open monitoring slowly reduces the frequency of automatic thoughts/ mind wondering.
What are the benefits of meditation?
Meditation has been shown to have both short-term (known as ‘states’) and long-term (known as ‘traits’) benefits.
They can be summarised as follows: (Ref)
1) Deep relaxation (body and mind)
2) Improved concentration/ attention span and better control of unwanted thoughts
3) Emotional wellbeing and stability, and better regulations of emotions
4) Improved resilience to stress (and adverse life events) and reduced stress symptoms
5) A balanced and positive attitude towards life.
Can meditation be used as a therapy?
Meditation has been an integral part of many religious/ cultural practices, wellbeing programmes/ Mind-Body techniques, such as Yoga, Tai chi, and Qigong.
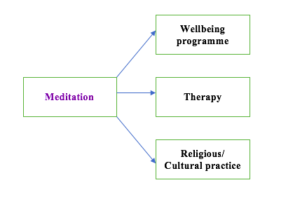
There is also a growing interest in meditation in the Western medicine both as a treatment and a complementary method (along with the ongoing conventional treatment).
For example, secular and standardised methods of mindfulness meditation have been developed to be used in clinical practice: (Ref)
1) Mindfulness-Based Stress Reduction (MBSR): for chronic pain, cancer, and migraine.
2) Mindfulness-Based Cognitive Therapy (MBCT): prevention of a relapse of depression episode.
3) Mindfulness-based Relapse Prevention/ Mindfulness-Oriented Recovery Enhancement:
for the treatment of substance misuse.
In summary, therapies based on meditation techniques have been used for the following:
2. Coping with chronic physical health problems, including pain.
3. Complementary treatment for psychiatric conditions, such as anxiety and depression.
What is the scientific basis for the meditation practices?
Numerous studies have been done to investigate the impact of meditation on the neurophysiology and other systems. Beneficial effects of meditation have been shown in many studies. However, the result varies among different types of meditations, as the practice varies quite significantly. Therefore, it is difficult to ascertain a ‘dose-effect’ relationship and draw definite conclusions.
Moreover, there are many variables/ bias in the studies, including the personality, personal beliefs (on the benefits of meditation), prior experience of meditation, and the mindset of the individuals undertaking meditation practices. Therefore, the results should be interpreted with caution when it is extrapolated to the wider population.
In general, the effects of meditation on human physiology are thought to be mediated through:
A) The changes in the brain functions
B) The effects on the immune system.
What impact does the meditation have on the brain functions?
Studies have shown that the practice of meditation leads to:
– Specific EEG changes (mainly Theta waves) in many parts of the brain. The Theta activity indicates a state of relaxation at rest (but awake).
– Increase in blood supply in certain regions of the brain. (Ref)
– Activation of some specific areas of the brain and nerve networks (connections between different parts of the brain).
– Neuroplastic changes
– Increased secretion of certain neurohormones and neurotransmitters.
A brief summary of the possible changes in the brain functions:
1) Stress response pathway:
Please find the detailed mechanism of stress response here.
In summary, the amygdala assesses the stressors and if it feels that there is a threat/ danger, then sends a signal to the hypothalamus to initiate a stress response (with the activation of the sympathetic nervous system and the HPA axis).
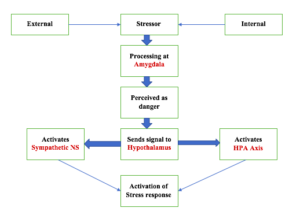
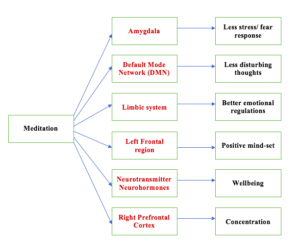
Meditation has been shown to reduce the activity of the amygdala in response to stress. (Ref)
Activation of the anterior cingulate and insula areas help in the reduced sympathetic activity (as they decrease the activation of the amygdala).
Therefore, meditation leads to a reduced activation of the Sympathetic nervous system/ HPA Axis. This, in turn, leads to an activation of the parasympathetic nervous system and maintaining homeostasis/ stability (both physical and mental).
As a result, meditation leads to reduced ‘Fight and Flight’ response and stress relief.
This has been proven by reduced heart rate, blood pressure, and less chemical markers (of sympathetic nervous system activation) in the urine (Vanillyl mandelic acid) and blood (cortisol and adrenaline). (Ref)
Reduced resilience to stress helps in the prevention of Blood Pressure related problems and heart diseases.
2) Theta wave on EEG:
Meditation activates following areas of the brain with the development of Theta waves in EEG:
1. The left frontal region of the brain (this area is related to positive feelings and emotions)
2. Frontal (prefrontal cortex and anterior cingulate cortex), mid and right central brain regions.
The Theta activity indicates a state of relaxation at rest (but awake).
3) Default Mode Network (DMN)
Meditation has been shown to reduce the activity of DMN. Gamma waves are found on EEG when the DMN is active. Research indicates reduced Gamma wave activity during meditation. (Ref)
This supports the concept of ‘thoughtless awakening’ during meditation.
What is the Default Mode Network (DMN)?
Researchers suggest that when we are not actively concentrating on something, our brain goes off into the Default Mode. During these times, our mind goes into an ‘autopilot mode’ and we experience ‘mind wandering’. Different thoughts come to our mind (both positive and negative) related to the past and future. Depending on the nature of the thoughts, we feel happy, sad or worried.
The areas of the brain which are involved in this automatic thought process are collectively called the Default Mode Network (DMN).
Therefore, the DMN is a group of separate (but closely connected) brain structures.
They are particularly active when we are awake but not actively concentrating on anything. The different brain structures which are thought to be a part of the DMN are:
– Medial prefrontal cortex
– Posterior Cingulate Cortex
– Inferior parietal lobe
– Lateral temporal cortex
– Temporoparietal junction
– Hippocampal formation
– Precuneus
3) Activation of neuronal networks:
Increased activity of fronto-parietal and fronto-limbic neuronal networks in the brain. This has been confirmed with Positron Emission Tomography (PET) scan.
These areas are related to increased concentration and regulations of the emotions.
4) The release of hormones:
Meditation leads to the release of hormones and neurotransmitters, such as Dopamine, Serotonin, and Melatonin, in the limbic system of the brain. They help in mood stabilisation, positive feelings, and a sense of wellbeing.
Melatonin is also known to boost the immune system.
5) Neuroplasticity:
Researchers have noted increased thickness of some brain structures (such as right middle and superior frontal cortex, and insula) with meditators.
Increased grey matter density has been also noted in the right insula, hippocampus, and left inferior temporal lobe.
The increased thickness of the right prefrontal cortex.
This area plays an important role in the concentration/ attention span.
What is neuroplasticity?
Neuroplasticity is the unique capacity of the brain to change in structure and function throughout the entire life (especially in response to training, experience, and injury). Therefore, the gray matter can become dense and new nerve networks (synapses) can develop in certain areas of the brain, if they are regularly activated.
On the contrary, if some brain areas remain less active, then they can shrink in size and the neural connections can fade away.
With the advancing age, the thickness of the cerebral cortex (gray matter) decreases. Meditation has been shown to increase the gray matter thickness. The process of neuroplasticity is thought to be responsible for this change.
What is the impact of meditation on the immune system? (1)
Stress is now thought to activate an inflammatory process in the body. Therefore, chronic stress can induce a state of chronic inflammation, which can contribute to many physical and mental health problems.
Research has shown that the meditation can reduce the inflammatory response. For example, chemical markers of the inflammation (such as Interleukin-6 (IL-6) and C-Reactive Protein), have been shown to decrease after the practice of meditation.
Mindfulness
This article on meditation would be incomplete without a brief discussion on mindfulness considering it’s growing popularity both in the healthcare sector and the corporate world.
What is mindfulness?
This is thought to be originated from Buddhism in 500 BC. However, researchers think that mindfulness might have originated several thousand years ago in India. (Ref)
The aim of mindfulness meditation is to keep the attention focussed at the current moment.
Then observing the thoughts coming to the mind without self-criticism.
Mindfulness, like other forms of meditation, also encourages to accept the thoughts/ events of life as they are (in a non-judgemental way).
Jon Kabat-Zinn first introduced mindfulness meditation as a clinical intervention in 1979. At the University of Massachusetts Medical School, he developed Mindfulness-Based Stress Reduction (MBSR) to treat long-standing pain symptoms. (2)
Subsequently, Mindfulness-Based Cognitive Therapy (MBCT) was developed. The aim of MBCT was to prevent recurrence of depression.
Mindfulness in pregnancy
In 1998, Nancy Bardacke formally introduced Mindfulness-Based Childbirth and Parenting (MBCP) to be used during the antenatal period.
MBCP is a class-based session (spread over usually 9 weeks) based on Mindfulness-Based Stress Reduction (MBSR) principles.
This encourages pregnant women (and partners) to apply mindfulness techniques to deal with fear, pain, physical and psychological stress (which may be associated with pregnancy, childbirth, postnatal period and challenges of parenting).
Mindfulness practice during pregnancy could be beneficial in the following ways:
1. Improvement of psychological wellbeing with a reduction in stress, anxiety, (antenatal and postnatal) depression.
2. Reduces pregnancy-related anxiety and fear of childbirth
3. Better parenting skills and emotional availability.
What are the risks of practicing meditation? (Ref)
There is a scarcity of studies looking at the adverse effects of meditation practices.
Meditation has been associated with the following adverse reactions:
– Disorientation and confusion
– Anxiety, delirium, insomnia, and hallucinations
– Psychosis (3)
– Post-traumatic stress disorders (PTSD)
– Epileptic attacks.
Therefore, people with physical/ mental health illnesses should get the necessary advice (from medical practitioners and meditation teachers) before starting any form of meditation.
Summary
1. The aim of meditative practices is to achieve a state of ‘thoughtless awareness’. This refers to a peaceful mind without any disturbing thoughts.
2. Meditation is a wakeful state and different from sleep.
3. Different forms of meditation practices exist. However, one basic common theme is concentration/ attentional focus.
4. Meditation is being used as a form of treatment in different health condition and stress management strategy.
5. Research indicates that meditation leads to certain changes in the function and structure (neuroplasticity) of the brain, both in short term and long term.
6. The practice of meditation/ mindfulness could be beneficial during pregnancy and the perinatal period.
7. People with physical/ mental health illnesses should get adequate advice from a healthcare practitioner and an experienced meditation teacher before commencing meditation practices. There are some scientific data and case studies to indicate possible potential risks with meditation practices.
Reference
1) Househam, Ayman & Peterson, Christine & Chopra, Deepak. (2017). The Effects of Stress and Meditation on the Immune System, Human Microbiota, and Epigenetics. Advances in mind-body medicine. 31. 10-25.
2) Kabat-Zinn, J., 1982. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen. Hosp. Psychiatry 4 (1), 33–47, http://dx.doi.org/10.1016/0163-8343(82)90026-3.
3. Walsh R, Roche L. Precipitation of acute psychotic episodes by intensive meditation in individuals with a history of schizophrenia. Am J Psychiatry. 1979 Aug; 136(8):1085-6.

