It is well known that the good nutrition during pregnancy is important for the growth and development of the baby and for fetal programming.
During pregnancy (and beyond), a healthy balanced diet (along with necessary nutritional supplements) is also important for good brain health and emotional wellbeing.
Nutritional neuroscience is an emerging topic to explore how mental health disorders can develop due to nutritional factors.
This article briefly outlines the role of nutrition for brain health, with special reference to pregnancy.
Nutrients are vital for the function of the brain.
To understand the role of the nutrition in the brain functions, it would be useful to discuss some basic neurophysiology.
For proper function of the brain and the nervous system, two essential and basic functions are necessary:
1. Synthesis of the neurotransmitters:
Neurotransmitters are also called the body’s chemical messengers. They are released from the end of the nerve cells to carry a nerve signal to the next nerve cell, muscle or any other structure.
A group of neurotransmitters, called ‘monoamine neurotransmitters’, plays a vital role in the mood and wellbeing of the individual.
There are three main neurotransmitters in this group: Serotonin, Noradrenaline, and Dopamine.
Mood disorders such as depression are associated with the deficiency or inadequate functioning of these neurotransmitters.
Serotonin is also important for memory, sleep, mood, and many different cognitive functions.
2. The proper function of the Cell membrane (the outer layer of each nerve cell):
Cell membranes ensure a balance of chemical signals entering into the cells, like a gatekeeper.
If the cell membranes do not function well, then the nerve cells become too permeable to the external chemicals. Therefore, they become very excitable, which can lead to mental health conditions and neurological illnesses.
Nutrition and brain function
Let us now consider which specific nutrients are required to carry out the above functions.
The synthesis of the monoamine and Acetylcholine neurotransmitters needs the following nutrients:
1. Amino acids: these are the building blocks of the proteins. Proteins in the diet, therefore, supply the amino acids. Some of the amino acids need to be supplied from the diet (as the body is unable to synthesise them). They are called essential amino acids.
Some important amino acids essential for the synthesis of neurotransmitters are Tryptophan, Tyrosine, and Methionine.
2. Vitamins: Folic Acid and Vitamin B12
3. Minerals: Zinc, Selenium, Magnesium, Iron
4. Choline
How do these nutrients maintain a good brain health?
Folic Acid and Vitamin B12
The amino acid Homocysteine would require Folic acid and Vitamin B12 to change to methionine. Methionine then changes to S-Adenosyl Methionine (SAM).
SAM is essential for the synthesis of monoamine neurotransmitters (Serotonin, Dopamine, and Nor-adrenaline) in the brain.
Vitamin B12 and Folic Acid supplementations have been shown to improve depression symptoms when used with antidepressants (when the initial response with SSRIs was poor).
Folate deficiency reduces the response to antidepressants. (Ref)
Zinc
The zinc adjusts the balance between the excitatory and inhibitory neurotransmission in the brain cells. Therefore, helps in modulating the brain’s excitability. (2)
It is also an important component of numerous enzymes of the body.
Zinc deficiency has been linked to depression, anorexia, impaired cognitive function, learning difficulties, epilepsy, and Alzheimer’s disease. (3)
People eating rice-based diets are more prone to develop Zinc deficiency. (4)
Deficiency of zinc has been described to be associated with increased severity of postnatal depression. (Ref)
There has been conflicting evidence from studies on using zinc supplements to prevent/ treat perinatal mental health conditions. While some studies recommended them (Ref) but others did not find them helpful. (Ref)
Zinc and Copper ratio (Ref)
The balance and the ratio of copper to zinc are more important for health than the concentration of either of these minerals.
Raised copper level and reduced Zinc level is one of the most common micronutrient imbalances in the human body.
This has been found in many health conditions, such as schizophrenia, depression, insomnia, autism, childhood hyperactivity, hypertension, fatigue, muscle and joint pain, headaches, and premenstrual syndrome.
It is recommended that pregnant women (or any adult) should take Zinc supplements if they are taking copper supplements (8 – 15 mg of zinc for every 1 mg of copper), because of a risk of imbalance of these two micronutrients
Magnesium
The magnesium prevents the entry of calcium in the nerve cells (therefore, acts as a ‘natural calcium channel blocker’). Calcium is known to excite the nerve cells. Therefore, magnesium has a calming effect on the nerve cells and the brain.
Magnesium deficiency can be caused by eating a diet less in magnesium or high in calcium and high level of stress hormones.
Magnesium supplement has been found to be effective in the treatment of depression.
Magnesium deficiency (along with excess calcium and stress) has been found to be associated with agitation, anxiety, irritability, confusion, asthenia, sleeplessness, headache, delirium, hallucinations, and hyperexcitability. (Ref)
Iron
Iron plays an important role in the healthy functioning of the brain by doing the following: (5)
1. Neurotransmitter synthesis:
Iron is a co-factor for some enzymes required for the synthesis of monoamine neurotransmitters, mainly serotonin, and dopamine.
2. Myelination:
For adequate myelination of white matter cerebellar folds and spinal cord, a good supply of iron is required.
Iron deficiency anaemia is very common during pregnancy.
Iron deficiency can lead to postnatal depression, impaired cognitive function, reduced attention span, and concentration. Studies have shown that depression and stress symptoms improve with iron supplementation. (6)
Selenium
Low selenium is known to increase the risk of preeclampsia and pregnancy-induced hypertension.
Studies have indicated that selenium supplementation might be able to prevent postnatal depression However, more research is required in this area.
Selenium helps in the synthesis of thyroid hormones. Selenium is a component of the enzymes that protect the brain cells from degenerations. (Ref)
Choline
This is a very important nutrient for the brain function. Choline is needed for the formation of the neurotransmitter, acetylcholine. This also helps in the synthesis of other neurotransmitters (as a ‘methyl group donor’). (7)
Dietary supply is required as the biosynthesis of choline is not enough to meet the increased requirement during pregnancy.
The recommended daily requirement of choline during pregnancy is 450mg/ day 9as compared to 425mg/ day for non-pregnant women). (8)
Rich source of choline are eggs, liver, chicken, fish, legumes, cruciferous vegetables, milk, and soya products.
Vitamin D
Vitamin D (also called the sunshine Vitamin) is produced in the skin with the exposure to ultraviolet rays from the sun.
Vitamin D, once produced in the skin, undergoes further changes (‘hydroxylation’) to become the active chemical (‘metabolite’). This is essential for the calcium metabolism in the body for healthy bones.
Research has indicated that Vitamin D could also be important to maintain healthy brain functions.
Vitamin D receptors and the hydroxylation enzymes (responsible for hydroxylation of inactive Vitamin D to change this to the active metabolite) have been found on different parts of the brain.
Studies have indicated an association between Vitamin D deficiency and mental health symptoms (such as depression, anxiety, and cognitive brain function).
Recent research has indicated that normal levels of Vitamin D in the blood could be protective of perinatal depression. (Ref)
Amino acids
Amino acids are essential for the synthesis of neurotransmitters in the brain and nervous system.
The requirement of amino acids increases during pregnancy. The essential amino acids are required to come from the diet as the body cannot synthesise them.
Healthy protein intake can ensure an adequate supply of amino acids.
Omega-3 Fatty Acids
Omega-3 fatty acids are a type of polyunsaturated fatty acids (PUFA). In a different note, the other variety of PUFA is Omega-6 fatty acids.
The omega-3 PUFA are essential fatty acids, i.e., they can not be synthesised in the human body. Therefore, they need to come from food. They are found in a variety of seafood, such as fish (salmon, tuna, sardines, cod, and anchovy) and algae. The other sources are vegetable oils, flax seeds, walnuts, and some types of vegetables.
They are vital for the baby’s brain and retinal development during pregnancy.
At the same time, omega 3 Fatty Acids are important for healthy brain function and prevention of perinatal depression.
Research has shown that pregnant women eating a low amount of seafood has more rate of antenatal depression. (Ref)
Also, a high intake of PUFA during pregnancy has shown to reduce the risk of postnatal depression. (9)
How Omega-3 fatty acids reduce the risk of depression/ mental health condition?
The exact mechanism is not known. It is thought to have two protective actions on the brain:
1. Reducing inflammatory process:
Inflammation is now thought to an important pathway for depression and other mental health conditions.
Omega-3 fatty acids are known to reduce the inflammatory process of the brain. For example, they reduce the synthesis of some chemicals (‘cytokines’) which initiate the inflammatory process. (10)
2. Reducing excitability of the nerve cells:
The omega-3 fatty acids undergo some changes (‘esterification’) within the outer membranes of the nerve cells of the brain. After the esterification, the PUFAs change into phospholipids within the cell membrane.
These phospholipids ensure the healthy function (‘fluidity’) of the cell membranes (11) and prevent the abnormal signals from entering the nerve cells (through ‘ion channel modulation’ (12), and ‘receptor mediation’ (13).
Low levels of omega-3 fatty acids have been shown to be linked with depression, suicidal ideations and negative thoughts/ attitude towards life. (14)
Is the requirement of omega-3 PUFA high during pregnancy?
The daily requirements of omega-3 PUFA increase in pregnancy.
As the omega-3 fatty acids are essential for the brain development of the fetus, they are transported from the mother’s blood to the fetus through the placenta. As a result, the blood levels of omega-3 fatty acids start to decline after the second trimester. It might take up to 6 months after the childbirth for the levels to return back to normal. (15)
As they can not be synthesised in the body, they need to be taken in adequate amount in the diet to prevent deficiency during pregnancy. Wome with omega-3 fatty acids can develop depression.
DHA is essential to brain growth and development in the fetus. As a result, maternal requirements for n-3 fatty acids are high. Maternal DHA status begins to decline in the second trimester and is ultimately depleted by the end of most pregnancies. DHA status does not return to its original level until over 6 months postpartum. (15)
As a result, women who do not supplement their diets with n-3 fatty acids are likely to develop DHA deficiency, which is associated with major depressive disorders. (16)
It is recommended that pregnant women should take at least 200 mg of DHA every day. 1 to 2 servings of seafood per week is enough to achieve this.
However, studies have found that fish consumption is usually much less. As a result, the growing fetus may be deficient the required amount of omega-3 PUFA. (Ref)
Why is seafood consumption restricted during pregnancy? (Ref)
The following toxins are found in the seafood:
– Mercury
– Polychlorinated biphenyls (PCBs)
They could be harmful to the developing fetus.
Therefore, it is recommended that the pregnant women should not take more than 2 servings of fish per week. This is equivalent to about 340 g or 12 oz of seafood per week.
Why are women prone to develop nutritional deficiency during pregnancy?
There is a risk of nutritional imbalance during pregnancy due to the following reasons:
A) High physiological demand: there is an increased requirement of the nutrition due to the need for the growing fetus and the physiological changes in the body (such as increased blood volume, growing uterus, and raised basal metabolic function).
B) Less food intake due to:
1. Nausea and vomiting in pregnancy/ hyperemesis gravidarum.
2. Aversion to food
C) Less availability of food due to poverty/ poor socio-economic conditions in many families around the world.
Why avoid excess food consumption during pregnancy?
The science and the traditional belief of the society often clash when it comes to eating during pregnancy.
Pregnancy is often seen as a time to let loose healthy dietary habits, with an intention to ‘eating for two’.
Women are often encouraged to allow weight gain freely.
In fact, many women (including obese women) describe the ‘pregnancy as a time when they finally are not judged for eating more than a modest portion and can gain weight freely without criticism’. (1)
Sometimes, excess food intake is a coping mechanism during stress.
Although the nutritional requirement increases during pregnancy, care has to be taken to avoid excessive weight gain during pregnancy.
Excess Gestational Weight Gain (GWG) could be detrimental to the health of the pregnant woman. This could increase the risk of gestational diabetes, preeclampsia, and venous thromboembolism.
Therefore, eating adequate (but healthy) food and exercise during pregnancy are important.
The summary of the recommendations from the World Health Organisation and Institute of Medicine (USA) on GWG are as follows:
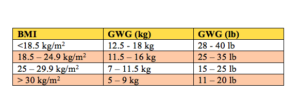
(WHO (2016) WHO recommendations on antenatal care for a positive pregnancy experience. World Health Organization, Geneva
Institute of Medicine. Dietary Reference Intakes: e Essential Guide to Nutrient Requirements. Washington DC: e National Academies Press; 2006)
Can cultural factors play any role in the nutrition during pregnancy?
In many parts of the world, many pregnant women do not get adequate nutrition due to poverty. Moreover, cultural beliefs and rituals play an important role in the food intake during pregnancy.
For example, in some Ghanian communities, pregnant women are not advised to eat meat and certain vegetable to avoid having a ‘spirited child’. (17)
In Tanzania and many parts of Africa, women are advised to avoid eating eggs during pregnancy. They fear that by eating eggs, animal characteristics could be transmitted to the baby. (Ref)
Cultural practices, values, and beliefs should be taken into account while advising pregnant women regarding food and nutrition.
Is consuming junk food safe during pregnancy?
The intake of junk/ fast food is increasing all over the world. This has now become a part of the busy lifestyle. These are often convenient, highly palatable and readily available, especially with the current era of Internet and food Apps in mobile devices. Advertising also plays a role in its popularity.
It is likely that the consumption of the fast food is also increasing in pregnant women. This trend is concerning as such food usually contain processed meat products, refined cereals, sweet drinks, and salty snacks.
They all could be health hazards (such as Type 2 diabetes, obesity, hypertension, abnormal lipid profile, and heart disease) if consumed in high quantity and for a long time. Moreover, the nutritional values are often lost in the processing and often, artificial coloring and preservatives are added too.
Research is emerging to show that fast food intake during pregnancy can influence fetal programming.
When this is consumed in high amount during pregnancy, the babies can become more prone to develop asthma, childhood obesity (with psychological consequences, such as low self-confidence and self-esteem, poor socialisation, and high rate of depression during childhood and adolescence)
Pregnant women consuming a high quantity of fast food are more likely to develop gestational diabetes
They also are at high risk of gain more weight during pregnancy with relevant consequences.
Unhealthy food consumption has been linked to more stress symptoms and depression.
Therefore, fast food is likely to have an impact on the mood and brain functions. However, more research is required to explore the impact of fast food on maternal mental health.
Therefore, it is advisable to avoid/ minimise the intake of fast food for a healthy lifestyle during pregnancy and beyond.
Can dietary interventions be helpful in the prevention and treatment of perinatal mental health conditions?
Some research has indicated that nutritional deficiency can increase the risk of depression both during pregnancy and postpartum.
Some nutritional interventions have been investigated as a preventative strategy (and treatment) for postnatal depression:
– Omega-3 (n-3) long-chain polyunsaturated fatty acids (LCPUFA)
– Vitamin D
– Overall diet.
Unfortunately, the studies in this regard lack consistency in their methodologies. Therefore, the exact role of the diet and nutrition in the development of the perinatal mental health disorders still remains inconclusive. (Ref)
Further research is required in this field to establish if any specific diet/ nutritional supplement can prevent/ treat mental health conditions during pregnancy/ postpartum. This could be a noninvasive and cost-effective intervention option for treatment.
Reference
1. Exploring knowledge and attitudes related to pregnancy and preconception health in women with chronic medical conditions. Chuang CH, Velott DL, Weisman CS. Matern Child Health J. 2010 Sep; 14(5):713-719. [PubMed]
2. Smart TG, Hosie AM, Miller PS. Zn2+ ions: modulators of excitatory and inhibitory synaptic activity. Neuroscientist. 2004;10:432–442.[PubMed]
3. Cunha MP, Machado DG, Bettio LEB, Capra JC, Rodrigues ALS. Interaction of zinc with antidepressants in the tail suspension test. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32:1913–1920. [PubMed]
4. Farzin L, Moassesi ME, Sajadi F, Amiri M, Shams H. Serum Levels of Antioxidants (Zn, Cu, Se) in Healthy Volunteers Living in Tehran. Biol Trace Elem Res. 2009;129:36–45. [PubMed]
5. Beard JL, Connor JR. Iron status and neural functioning. Annu Rev Nutr. 2003;23:41–58. [PubMed]
6. Beard JL, Hendricks MK, Perez EM, Murray-Kolb LE, Berg A, Vernon-Feagans L, et al. Maternal iron deficiency anemia affects postpartum emotions and cognition. J Nutr. 2005;135:267–272. [PubMed]
7. Zeisel SH. Choline: an essential nutrient for humans. Nutrition. 2000;16:669–71. [PubMed]
8. Institute of Medicine, and National Academy of Sciences USA. Dietary reference intakes for folate, thiamin, riboflavin, niacin, vitamin B12, panthothenic acid, biotin, and choline. National Academy Press; Washington DC: 1998. pp. 402–4.
9. Makrides M, Gibson RA, McPhee AJ, et al. DOMInO Investigative Team, authors. Effect of DHA supplementation during pregnancy on maternal depression and neurodevelopment of young children: a randomized controlled trial. JAMA. 2010;304:1675–1683. [PubMed]
10. Owen C, Rees AM, Parker G. The role of fatty acids in the development and treatment of mood disorders. Curr Opin Psychiatry. 2008;21:19–24. [PubMed]
11. Nakamura M, Nara T (2004) Structure, function, and dietary regulation of delta6, delta5, and delta9 desaturases. Annu Rev Nutr 24: 345–376. [PubMed]
12. Kang J, Leaf A (1996) Antiarrhythmic effects of polyunsaturated fatty acids. Recent studies. Circulation 94: 1774–1780. [PubMed]
13. Russell F, Burgin-Maunder C (2012) Distinguishing health benefits of eicosapentaenoic and docosahexaenoic acids. Mar Drugs 10: 2535–2559. [PubMed]
14. Desari AK, Grossberge GT. Herbal and botanicals in geriatric psychiatry. Am J Geriater Psychiatry. 2003;11:498–506. [PubMed]
15. Al M, van Houwelingen AC, Hornstra G. Long-chain polyunsaturated fatty acids, pregnancy, and pregnancy outcome. Am J Clin Nutr. 2000;71(1 Suppl):285S–291S. [PubMed]
16. Rechenberg K, Humphries D. Nutritional interventions in depression and perinatal depression. Yale J Biol Med. 2013 Jun 13;86(2):127-37. Print 2013 Jun. (Pubmed)
17. Arzoaquoi SK, Essuman EE, Gbagbo RY, Tenkorang EY, Soyiri I, Laar AK. Motivations for food prohibitions during pregnancy and their enforcement mechanisms in a rural Ghanaian district. J Ethnobiol Ethnomed. 2015;11:59.

