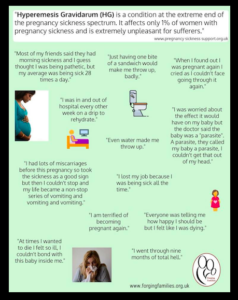
Hyperemesis Gravidarum (HG) is a debilitating illness affecting 1 in 10 women during pregnancy. This could have a profound impact on the physical health and psycho-social wellbeing of the woman. This article gives an overview of this health condition and advocates for a holistic approach to the care of HG.
How common are nausea and vomiting in pregnancy?
Nausea and/ or vomiting during pregnancy (NVP) is very common affecting about 7 out of 10 women during pregnancy.
NVP can happen any time of the day and not only in the morning. Therefore, the term, ‘morning sickness’, is a misnomer.
The symptoms typically start between the 4th and 7th week of pregnancy, peaks in around the 9th week and resolve by the 20th week in 90% of women. (Ref 1)
For the majority of the women, the symptoms are mild and self-limiting.
What is Hyperemesis Gravidarum (HG)?
When a pregnant woman suffers from severe symptoms of nausea and vomiting, then this is called hyperemesis gravidarum (HG). This occurs in 1 in 100 women during pregnancy.
This could require frequent, multiple and/ or prolonged hospital admission.
A diagnosis of HG is made when all other causes of nausea and vomiting have been ruled out. However, there is no single accepted clinical definition of HG (Ref 2).
A clinical diagnosis of HG is made when there are severe nausea and vomiting (in absence of any other cause of nausea and vomiting) along with:
– Weight loss: greater than 5% of the pre-pregnancy weight
– Dehydration
– Electrolyte imbalance in the blood
Women with HG could also have the other symptoms such as excessive salivation (‘Ptyalism’), a heightened sense of smell and incontinence of urine. Moreover, dehydration can cause a headache and constipation.
How can you measure the severity of NVP?
The Royal College of Obstetricians and Gynaecologists (UK) recommends the use of a validated scoring system, such as Pregnancy-Unique Quantification of Emesis (PUQE) score.
The International Classification of Disease (ICD – 10) (World Health Organization 2004) classifies HG as:
– Mild: HG starting before the end of 22 weeks without metabolic disturbances.
– Severe: HG starting before the end of 22 weeks with metabolic disturbances (Carbohydrate depletion, dehydration, and electrolyte imbalance).
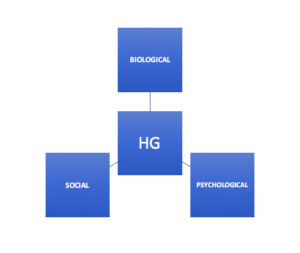
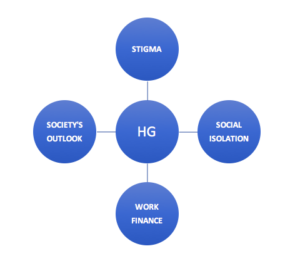
Bio-Psycho-Social impact
What are the impacts of Hyperemesis Gravidarum?
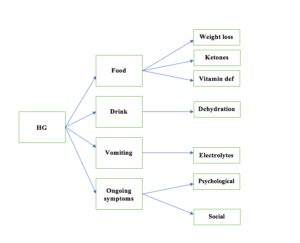
A) Biological:
Due to severe nausea and vomiting, the woman is unable to tolerate food and/ or fluid. As a result, the body goes through the changes of acute starvation:
Lack of food intake leads to carbohydrate depletion, which usually manifests as ketones in the urine, weight loss and vitamin deficiency (especially Vitamin B1 or Thiamine).
Lack of fluid leads to symptoms of dehydration (such as feeling weak, unable to stand, headache). Prolonged dehydration and lack of mobility increase the risk of blood clots (venous thromboembolism).
B) Psychological:
Significant impact on the quality of life and emotional health and wellbeing
C) Social:
This could lead to social isolation and sickness at work.
What are the impacts of HG on the emotional health and wellbeing?
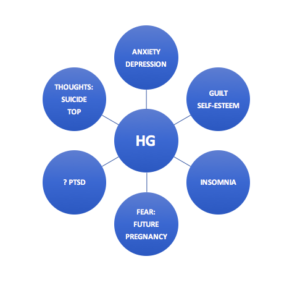
A) Mental health conditions (Ref 3)
– Women with Hyperemesis Gravidarum are at increased chance of developing anxiety and depression, both during the pregnancy and after the childbirth.
– There are some studies to suggest that they can also suffer from Post-Traumatic Stress Disorder (PTSD).
– The mental health symptoms can continue even after nausea/ vomiting has stopped.
B) Insomnia
NVP/ HG can cause sleep disturbance/ insomnia. This could lead to anxiety/ depression.
C) Lack of self-esteem and guilt: (Ref 4)
These can happen due to the following –
Self-care:
They might be unable to carry out day-to-day activities themselves and have to depend on others: showering, brushing their teeth and hair or getting dressed, eating or preparing food, and standing up without assistance.
Household chores and childcare:
Often, the woman is unable to carry out household chores such as cooking for the family and childcare responsibilities due to their ongoing illness.
There is a belief among many that HG is a part of pregnancy symptoms and not an illness. As a result, there is often very unrealistic expectation from the woman. This includes every part of her roles, such as a member of the family, mother, wife, employee or the wider society. (Ref 4)
D) Thoughts of termination of pregnancy and suicide: (Ref 4)
She could get persistent negative thoughts due to severe ongoing symptoms. As a result, she could feel that she is unable to cope any more.
E) Future pregnancy: (Ref 4)
She could avoid considering another pregnancy in the future due to the fear of recurrence of HG.
 Impact on Psychological wellbeing
Impact on Psychological wellbeing
What are the impacts of Hyperemesis Gravidarum on the social life of the woman?
A. Social isolation:
Persistent HG symptoms could lead to the social isolation of the woman due to the following:
1) Fear of humiliation in the public places/ social gatherings due to uncontrolled vomiting
2) To avoid contact with people who could make judgemental comments or question the severity of the condition. Sadly, there is often lack of awareness in the society.
3) To avoid the aggravation of symptoms from external sensory stimulation.
B. Loss of earning and job
Can pre-pregnancy mental health conditions predispose to HG? (Ref 5)
Historically it has been believed that HG is a manifestation of underlying or pre-existing mental health conditions.
However, all the recent studies indicate that this is not the case. In other words, HG is not caused by any underlying or pre-existing psychiatric illness.
HG is now considered to be a separate clinical entity and health condition without any known cause.
In spite of that, many healthcare professionals still try to explore and establish psychiatric conditions, when women present with HG. Recent studies have recommended that such clinical practice is of no value.
In fact, HG can lead to psychological conditions mentioned above.
Why do some women not seek help early?
This can happen due to the following reasons:
Stigma
People from many parts of the world (including some healthcare professionals) believe that the HG is a psychiatric condition. As a result, HG is often associated with stigma in the society.
Safety of drugs
Many women feel that it is not safe to take any medication during early pregnancy.
Every pregnant woman should be reassured that there are many safe medications available to treat HG.
I do not have HG. Is this a sign that my pregnancy is not going well?
There is a belief among many that absence of NVP/ HG is a sign of failing pregnancy. They feel that NVP/ HG is related to high levels of pregnancy hormones.
As a result, many women feel reassured when they develop nausea/ vomiting. This is especially true for women who had previous miscarriage or stillbirth.
However, there is no evidence to suggest that NVP/ HG is directly correlated with the pregnancy hormone levels. Therefore, healthy pregnancy is possible without NVP/ HG.
The exact cause of NVP/ HG is not known.
A holistic approach to care in HG
A comprehensive and holistic approach to the care is paramount to reduce her endless sufferings.
Along with the treatment of physical symptoms, adequate care should be taken to address her psychological and social needs.
A sensitive and understanding approach is required by the healthcare professionals.
The treatment of HG often remains confined to the treatment of the physical symptoms (such as the treatment of nausea/ vomiting and correcting dehydration and nutritional deficiency). It may be necessary to arrange Psychological counselling or a referral to the perinatal mental health team to treat her anxiety/depression.
“The woman’s perception of the severity of her symptoms plays a critical role in the decision of whether, when, and how to treat nausea and vomiting of pregnancy.”(Ref 2).
It may be necessary to arrange Psychological counselling or a referral to the perinatal mental health team to treat her anxiety/depression.
Peer support could play an important role.
With adequate care, an excellent outcome is possible.
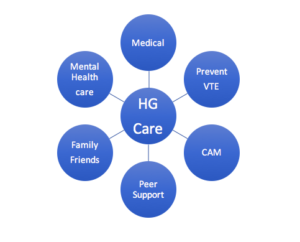
Holistic care
What else could be helpful apart from medications to treat HG? (Ref 2)
1. Dietary changes:
– Avoiding full stomach by having small meals every 1-2 hours, instead of large meals on long intervals.
– Avoiding spicy or fatty food
– Avoiding Iron supplements (to substitute Folic acid for Iron supplements)
– Eating bland and dry food and high-protein snacks
– Eating crackers in the morning before getting out of the bed.
2. Taking adequate rest
3. Avoid stimuli:
Some sensory stimuli could precipitate nausea/ vomiting. Therefore it could be helpful to identify the stimuli and avoid them. This could include strong smell, heat, humidity, noise and flickering/ flashing lights.
4. Ginger
5. Complementary and Alternative Medicine (CAM):
Acupressure/ Acupuncture could be helpful
Courtesy: Rachel Gardner. Forging Families (UK)
Is it possible to prevent HG?
It may not be possible to entirely prevent the occurrence of HG, as the exact cause of this is unknown.
However following could be helpful:
1. Prenatal multivitamin:
Taking multivitamin supplements, especially those containing Vitamin B 6 (Pyridoxine), at least 1 month before conception may reduce the risk of HG. The exact mechanism is not known. However, Pyridoxine is thought to improve nausea/ vomiting. This is sometimes used to treat NVP/ HG. (Ref 2)
2. Treatment of NVP:
Early appropriate treatment of NVP may prevent the progression to HG. (Ref 2)
Summary and key points:
– HG is a debilitating illness affecting 1 in 100 pregnant women.
– This could have a significant negative impact on the quality of life and physical, psychological and social wellbeing.
– HG is not a psychiatric illness nor caused by any pre-existing mental health condition.
– Good treatment is available.
– A comprehensive and holistic approach is vital, taking into account her psychological and social needs.
– Peer Support, such as Pregnancy Sickness Support (UK), could play an important role in the entire journey.
Further information on HG:
1. Pregnancy Sickness Support (UK)
2. RCOG Green Top Guideline (UK)
3. NHS Choices
Reference
1. Einarson A, Maltepe C, Boskovic R, Koren G. Treatment of nausea and vomiting in pregnancy: an updated algorithm. Can Fam Physician 2007;53:2109–11.
2. ACOG Practice Bulletin No. 189: Nausea And Vomiting Of Pregnancy. January 2018.

