Insomnia during pregnancy is very common. Research indicates that treatment of sleep disturbances during pregnancy can reduce many pregnancy and birth complications, and also antenatal and postnatal depression. This article outlines the incidence, causes and treatment of insomnia during pregnancy and beyond.
How many hours of sleep a pregnant woman needs?
An adult should have 7 – 9 hours of sleep. A pregnant woman might require some more hours of sleep every night or short naps in the daytime.
This is especially important when the mother is feeling tired and exhausted.
During the pregnancy, the woman’s body undergoes many changes. Some of the organs, such as heart, work much harder. Therefore, some extra hours of sleep are beneficial.
What is insomnia?
Insomnia or sleeplessness is a condition when someone is finding it difficult to fall asleep or waking up from sleep very early. This could also be associated with a feeling of unrefreshing sleep (also called ‘Non-Restorative sleep’), (Ref 1)
How common is insomnia during pregnancy?
Sleep disturbances are common during pregnancy.
During a survey by the US National Sleep Foundation (1998), 78% of women reported disturbed sleep during their pregnancies. (Ref 2)
Interestingly, studies have found that women sleep more (‘hypersomnolence’) during the first trimester. This is thought to be related to the rising levels of the hormone progesterone. Therefore, the insomnia is lowest during this time. Subsequently, insomnia worsens as the pregnancy advances. (Ref 3)
Insomnia in pregnancy is worst during the third trimester. (Ref 4)
Sleep disturbances continue to worsen for the first 6 months after the delivery. (Ref 5)
Moreover, women sometimes do not get adequate time to sleep leading to sleep deficiency. This is especially common after the baby is born. Usually, this improves once the baby’s circadian rhythm matures and regular sleep routine develops.
Does the quality of sleep changes during pregnancy?
Apart from insomnia, the quality of sleep also deteriorates during pregnancy and postpartum period. This worsens as the pregnancy advances. (Ref 6)
There are two main stages of sleep: Non-Rapid Eye Movement (NREM) and the Rapid Eye Movement (REM). These two stages alternate during the entire sleeping time.
NREM stages 3 and 4 (deep sleep) are important to feel refreshed after the sleep. During these stages, the brain activity is the lowest. On the other hand, the brain activity is the highest during the REM stage.
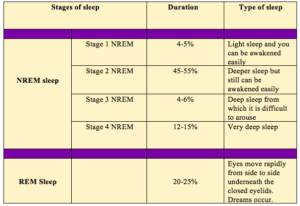
During the pregnancy, there is an increased duration of the Stage 1 NREM sleep and a reduction of Stage 3 and REM sleep. (Ref 7)
As a result, the total duration of the sleep is shorter. This is associated with frequent awakening and a longer wake period. (Ref 8)
The quality of sleep could be impaired further if there is sleep apnoea. (Ref 9)
Finding a comfortable sleeping position could be also challenging, especially during the latter half of the pregnancy.
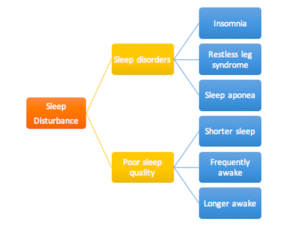
What are the common Sleep disturbances during pregnancy?
A. Sleep disorders:
1. Insomnia
2. Sleep apnoea
3. Restless leg syndrome
B. Reduced quality of sleep:
1. Shorter sleep duration
2. Increased awakening
3. Longer wake period
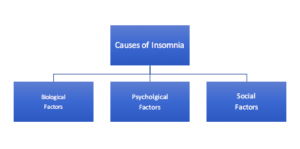
What are the causes of insomnia during pregnancy?
The exact cause of insomnia during pregnancy is unknown. However, the following are the contributory factors:
A. BIOLOGICAL FACTORS
1. Pregnancy changes/ conditions:
– First Trimester: fatigue, nausea, vomiting
– Second and third trimester: physical discomfort due to the growing fetus, backache/ SPD, increased urinary frequency, baby’s movement, breast tenderness, leg cramps, heartburn/ Gastroesophageal Reflux Disease (GERD).
2. Hormonal factors:
– Progesterone causes daytime sleepiness but night time fragmented sleep.
– Oxytocin (the hormone responsible for uterine contractions) secretion increases at night. Oxytocin causes sleep disturbance by creating a hyper-arousal state.
– Rising cortisol level could also cause the hyper-alert state.
3. Sleep disorders:
Other associated sleep disorders could aggravate insomnia, such as Restless Leg Syndrome and Sleep Apnoea.
B. PSYCHOLOGICAL FACTORS
1. Psychological stress: Worries about the labour, childcare, work/ financial issues.
2. Mental health conditions: Common mental health conditions (such as anxiety, depression, OCD, Bipolar illness, PTSD) are often associated with insomnia.
C. SOCIAL FACTORS
Lack of social support, relationship problems, poor housing conditions.
Can insomnia lead to pregnancy and birth complications?
Chronic insomnia can cause certain pregnancy and birth complications mentioned below. (Ref 10)
However, these complications are rare and do not happen to every mother with sleep disturbance. Therefore, mothers with insomnia should not be unnecessarily alarmed.
1. Quality of life: Daytime sleepiness, fatigue, lack of concentration
2. Family relationship:
– Relationship problems with the partner
– Bonding and attachment difficulties
3. Pregnancy complications: Gestational Diabetes, Preeclampsia, Preterm birth, fetal growth restriction
4. Labour: Increased pain during labour, increased duration of labour, increased Caesarean birth
5. Mental health conditions: Antenatal depression, Postnatal depression

How insomnia during pregnancy causes postnatal depression?
Insomnia is a risk factor for both antenatal and postnatal depression. (Ref 11) However, no one knows the exact mechanism of how this happens.
Scientists think that insomnia initiates a stress response in the body. This also leads to release of certain inflammatory markers (‘Cytokines’) in the blood (such as Interleukin 6). (Ref 12)
Such Cytokines are found in a higher level in mothers with postnatal depression, preterm birth, and certain other pregnancy complications.
This stress-related inflammatory pathway could be an explanation of how insomnia causes depression. However, further research is required to confirm this pathway.
What is Sleep Apnoea?
This is a sudden cessation of breathing or a period of very shallow breathing during sleep. Sleep apnoea can last for few seconds to minutes. This could happen several times during the sleep.
Obstructive sleep apnoea (OSA) happens due to narrowing of the air passage. This leads to obstruction to the breathing and results in sleep apnoea.
OSA occurs more commonly in pregnant mothers (10-25%) compared to non-pregnant women (2%). (Ref 13)
Factors during pregnancy which contribute to the OSA are:
– Weight gain
– Elevation of the respiratory muscle, diaphragm, due to the growing fetus.
– Swelling (oedema) of the linings of the nose (nasal mucosa) and air passage (pharyngeal mucosa) due to the high level of oestrogen. This leads to obstruction to breathing, resulting in OSA.
Treatment of OSA:
CPAP (Continuous Positive Airway Pressure) is an effective treatment of OSA. This is very safe during pregnancy.
What is Restless Leg Syndrome (RLS)?
This is a nerve condition where a person has irresistible urge to move the legs. It could be related with very uncomfortable creeping and crawling sensation in the legs and feet, especially in the evening and night. This leads to severe disturbance of sleep.
RLS occurs more commonly in pregnant mothers (27-30%) (Ref 14) compared to non-pregnant women (3.4-10%).
RLS can deteriorate as the pregnancy advances, being worse in the third trimester. (Ref 15)
RLS usually resolves itself after the baby is born. Clinicians often underdiagnose RLS due to the lack of awareness of this condition. RLS is often thought to be the leg cramps, which are very common pregnancy symptoms.
Sometimes, the RLS is related to iron deficiency anaemia and folate deficiency. These can lead to the impaired function of the neurotransmitter, Dopamine. This, in turn, could lead to neurological symptoms of RLS.
Therefore, dietary iron and folic acid supplementation could help to treat RLS.
What is the treatment of insomnia?
Sleep hygiene is very important in dealing with insomnia. However, medications may be required for the treatment in some cases.
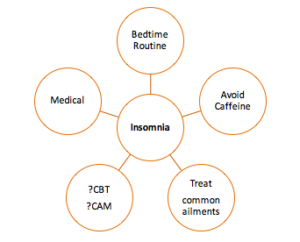
What can I do to maintain a good sleep hygiene?
– Healthy bedtime routine: You should have a certain time in going to bed every night and waking up in the morning. This helps the biological clock of the body to work more effectively. Sometimes warm bath before the bedtime could be useful.
– Try to avoid a daytime nap, if you are having difficulty to sleep at night.
– Avoid taking a caffeine-containing drink (tea, coffee, cola drinks), especially before the bedtime.
– Avoid drinking too much fluid in the late evening or before bedtime. This would reduce the frequency of getting up at night to pass need to pass urine. Therefore, this would help in less disruption of the sleep.
– Avoid watching television, long hours of work on computer or phone before the bedtime.
– Reading books and listening to soothing music at the bedtime could help.
– Avoid strenuous exercise/ workout in the late afternoon or evening.
– Finding a comfortable sleeping position would be helpful. Sometimes this could be achieved through the use of extra pillows or special maternity pillows.
Can complementary and alternative medicine (CAM)/ relaxation techniques help in treating insomnia?
The practice of yoga, meditation, mindfulness, acupuncture, massage, reflexology could be helpful. However, more research is required in this field to provide recommendations. (Ref 16)
What else could be helpful?
1. Treatment of heartburn/ reflux disease: avoid spicy food, especially in the evening. Sometimes over-the-counter antacids could be helpful. However, always check with the pharmacist/ doctor that they are safe to be taken during pregnancy.
2. Physical discomfort/ backache: Local application of heat and supportive pillows could be helpful.
3. SPD/ Carpal Tunnel syndrome: It could be helpful to get advice from a physiotherapist
Can medication be helpful in treating insomnia during pregnancy?
Promethazine
NICE Guideline (UK) suggests considering Promethazine if the mother is having ‘severe or chronic sleep problem’
Benzodiazepines
These are the group of medications commonly used to treat insomnia in non-pregnant mothers. However, they are preferably avoided during pregnancy. Studies have shown that benzodiazepines could cause “floppy infant syndrome” if the mothers are taking them for a long time. This could also lead to neonatal withdrawal symptoms.
Briggs GG, Freeman RK, Yaffe SJ. Drugs in pregnancy and lactation: a reference guide to fetal and neonatal risk, 9th ed Philadelphia: Lippincott Williams & Wilkins, 2011, pp. 401–401.
Antidepressants
Antidepressants are used for the treatment of associated depression. However, the mother should be given appropriate information on the use of antidepressants during pregnancy. Antidepressants are usually not used to treat insomnia alone.
Can the psychological treatment be helpful?
Cognitive Behavioural Therapy (CBT) has been found effective in the treatment of insomnia in non-pregnant women. However. the data is limited for the use of CBT in pregnancy to treat insomnia.
This could be effective if the insomnia is associated with anxiety or depression.

Conclusion
Good sleep is vital for healthy pregnancy outcomes, both for the mother and the baby. However, the sleep disturbances are often not appropriately addressed during pregnancy. This might be due to a lack of awareness among healthcare professionals. Insomnia could lead to some pregnancy, birth and perinatal mental health conditions. However, every pregnant mother must be reassured that such complications/ condition does not occur in every pregnancy. It is possible to treat insomnia during pregnancy successfully.
References
1. American Academy of Sleep Medicine. International classification of sleep disorders: diagnostic and coding manual, 2nd ed Westchester, IL: American Academy of Sleep Medicine, 2005
2. National Sleep Foundation (1998). Poll on Women and Sleep. National Sleep Foundation, Washington DC.
3. Schweiger MS. Sleep disturbance in pregnancy: a subjective review. Obstet Gynecol 1972, pp. 879–882. [PubMed]
4. Nodine PM, Matthews EE. Common sleep disorders: management strategies and pregnancy outcomes. J Midwifery Womens Health. 2013;58(4):368–377. [PubMed]
5. Shinkoda H, Matsumoto K, Park YM. Changes in sleep-wake cycle during the period from late pregnancy to puerperium identified through the wrist actigraph and sleep logs. Psychiatry Clin Neurosci. 1999;53(2):133 –5. http://dx.doi.org/10.1046/j.1440-1819.1999.00518.x. [PubMed]
6. Orff HJ, Meliska CJ, Lopez A, Martinez F, Sorenson D, Parry BL. Polysomnographic evaluation of sleep quality and quantitative variables in women as a function of mood, reproductive status, and age. Dialogues Clin Neurosci. 2012;14(4):413–424. [PubMed Central][PubMed]
7. Brunner DP, Münch M, Biedermann K, Huch R, Huch A, Borbély AA. Changes in sleep and sleep electroencephalogram during pregnancy. Sleep. 1994;17(7):576–582. [PubMed]
8. Wilson DL, Barnes M, Ellett L, Permezel M, Jackson M, Crowe SF. Decreased sleep efficiency, increased wake after sleep onset and increased cortical arousals in late pregnancy. Aust N Z J Obstet Gynaecol. 2011;51(1):38–46. [PubMed]
9. Franklin KA, Holmgren PA, Jönsson F, Poromaa N, Stenlund H, Svanborg E. Snoring, pregnancy-induced hypertension, and growth retardation of the fetus. Chest. 2000;117(1):137–141. [PubMed]
10. Chang JJ, Pien GW, Duntley SP, Macones GA. Sleep deprivation during pregnancy and maternal and fetal outcomes: is there a relationship? Sleep Med Rev. 2010;14(2):107–114.doi:10.1016/j.smrv.2009.05.001. [PMC free article] [PubMed]
11. Skouteris H. Germano C. Wertheim EH. Paxton SJ. Milgrom J. Sleep quality and depression during pregnancy: A prospective study. J Sleep Res. 2008;17:217–220. [PubMed]
12. Okun ML, Coussons-Read ME. Sleep disruption during pregnancy: how does it influence serum cytokines? J Reprod Immunol. 2007;73:158–65. [PubMed]
13. Nodine PM, Matthews EE. Common sleep disorders: management strategies and pregnancy outcomes. J Midwifery Womens Health. 2013;58(4):368–377. [PubMed]
14. Manconi M, Govoni V, De Vito A, Economou NT, Cesnik E, Casetta I, et al. Restless legs syndrome and pregnancy. Neurology. 2004;63(6):1065–1069. doi:10.1212/01.wnl.0000138427.83574.a6.[PubMed]
15. Wilt TJ, MacDonald R, Ouellette J, Khawaja IS, Rutks I, Butler M, et al. Pharmacologic therapy for primary restless legs syndrome: a systematic review and meta-analysis. JAMA Intern Med. 2013;173(7):496–505. doi:10.1001/jamainternmed.2013.3733. [PubMed]
16. Hollenbach D, Broker R, et al. Non-pharmacological interventions for sleep quality and insomnia during pregnancy: a systematic review. J Can Chiropr Assoc 2013; 57: 260–270. [PMC free article] [PubMed]
Photo credit

